BPH vs. Prostate Cancer
When it comes to men’s health, two common conditions that often cause concern are Benign Prostatic Hyperplasia (BPH) and prostate cancer. While they both involve the prostate gland, it’s important to understand the key differences between the two conditions. In this blog post, we will explore the differences between BPH and prostate cancer, including their causes, symptoms, and treatments.
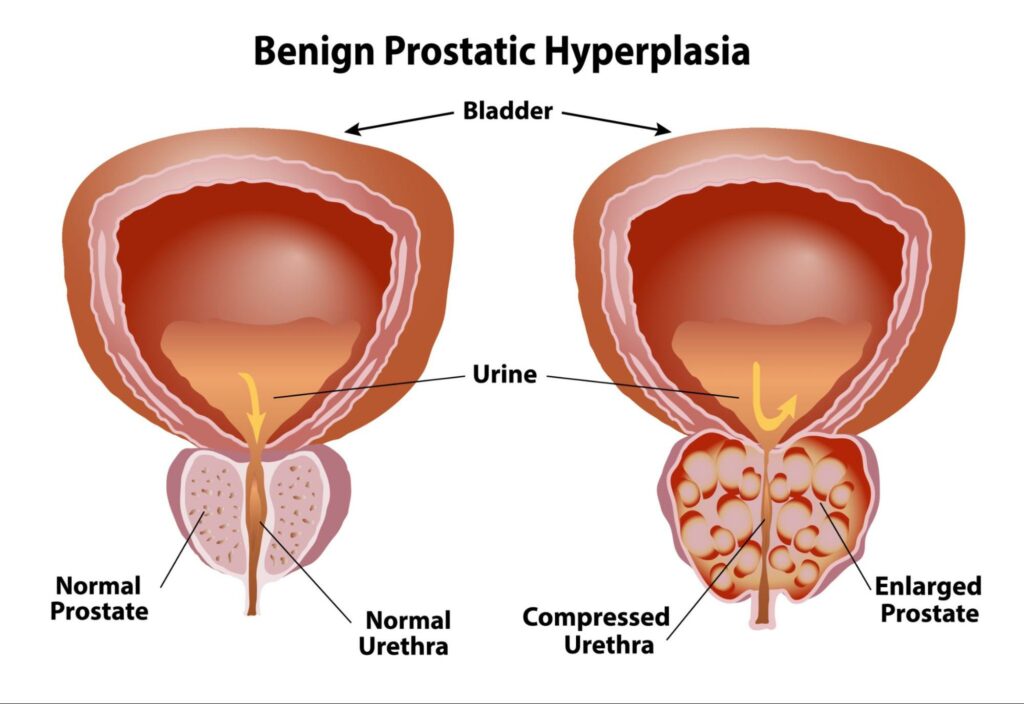
Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia, commonly known as BPH, is a non-cancerous enlargement of the prostate gland. The prostate is a walnut-sized gland located below the bladder and surrounds the urethra, the tube through which urine passes. As men age, the prostate often grows larger, leading to BPH.
Causes of BPH
The exact cause of BPH is not fully known, but it is believed to be primarily influenced by hormonal changes associated with aging, particularly the increase in dihydrotestosterone (DHT) levels.
Symptoms of BPH
Symptoms of BPH are related to the enlargement of the prostate gland and can include urinary problems such as the following:
- Frequent urination, especially at night
- Urgency to urinate
- Weak or interrupted urine stream
- Difficulty starting or stopping urination
- Inability to completely empty the bladder
Diagnosis and Treatment of BPH
Some doctors may use the same tests to diagnose BPH and prostate cancer, but other tests can help confirm you have BPH. Here are a few tests that your doctor may use to diagnose you:
- PSA Blood Test – The PSA (Prostate-Specific Antigen) Blood Test is a screening tool used to measure the levels of a protein produced by the prostate gland in the bloodstream. Elevated PSA levels can indicate BPH.
- Digital Rectal Exam (DRE) – A DRE is a physical exam that assesses the prostate gland’s size, shape, and texture. The doctor can feel for any enlargement that may be a sign of BPH.
- Urinary Flow Test – A urinary flow test assesses the rate and pattern of urine flow during urination, which helps determine if your bladder is efficiently emptying and detects any urinary obstructions that can be a sign of prostate enlargement.
- Transrectal Ultrasound (TRUS) – TRUS is an imaging test that creates detailed images of the prostate gland to assess its size and detect any abnormalities in the prostate.
Treatment for BPH depends on the severity of your symptoms, the size of the prostate, and your overall health. Here are some treatments to help with BPH:
- Alpha-Blockers: These medications relax the muscles in the prostate, improving urinary flow and reducing symptoms such as difficulty starting urination and weak urine stream.
- 5-alpha-Reductase Inhibitors: These medications shrink the prostate gland by reducing the production of dihydrotestosterone (DHT), a hormone that contributes to prostate growth.
- Prostate Artery Embolization (PAE): PAE is a minimally invasive procedure that involves blocking the blood supply to the prostate gland, causing it to shrink and relieve urinary symptoms. PAE is a better option for men who are not candidates for surgery or prefer a less invasive approach.
- Prostatic Urethral Lift (UroLift): UroLift involves placing small implants in the prostate to lift and hold the enlarged tissue away from the urethra, improving urine flow and reducing BPH symptoms.
- Transurethral Resection of the Prostate (TURP): TURP is a traditional surgical procedure used to remove excess prostate tissue obstructing the urethra.
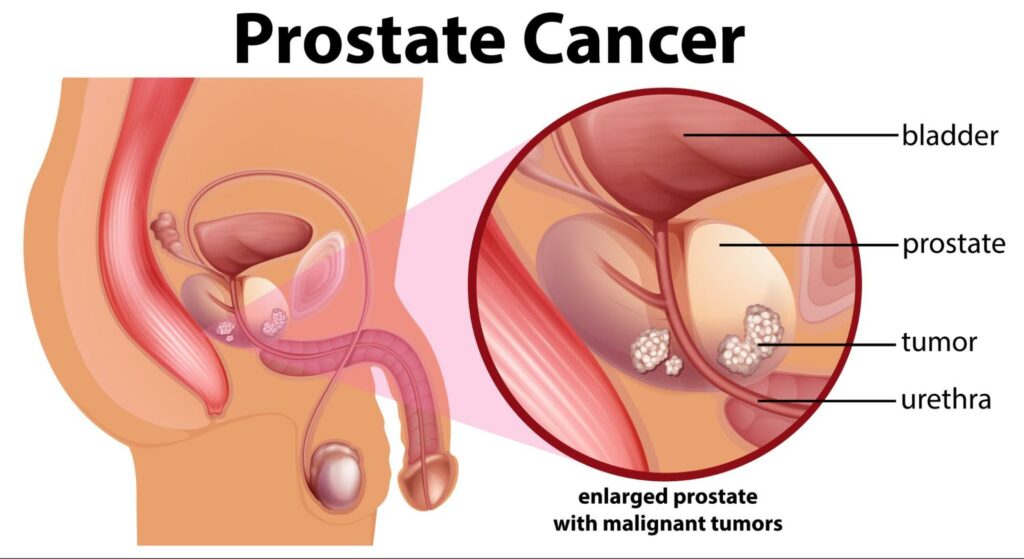
Prostate Cancer
Prostate cancer, on the other hand, is the abnormal growth of cells within the prostate that can invade nearby tissues and spread to other parts of the body. Unlike BPH, prostate cancer is a more serious condition that requires prompt diagnosis and treatment.
Causes of Prostate Cancer
- Age (risk increases with age)
- Family history of prostate cancer
- Race (African-American men have a higher risk)
- Certain genetic factors
Symptoms of Prostate Cancer
In the early stages, prostate cancer may not cause noticeable symptoms. As the cancer progresses, symptoms may include the following:
- Difficulty urinating
- Blood in the urine or semen
- Erectile dysfunction
- Bone pain (in advanced stages)
Diagnosis and Treatment of Prostate Cancer
Detecting prostate cancer early is critical for successful treatment. Some of the diagnostic tools that are is
- PSA Blood Test: A prostate-specific antigen test measures the level of a protein produced by the prostate, which can help detect prostate cancer.
- Digital Rectal Exam (DRE): A digital rectal exam (DRE) is a physical exam that allows healthcare providers to check the size, shape, and condition of the prostate gland.
- Biopsy: If prostate cancer is suspected, a biopsy is performed to confirm the diagnosis.
Treatment options for prostate cancer vary depending on the stage and aggressiveness of the cancer:
- Active Surveillance: A proactive approach to managing low-risk prostate cancer where patients are closely monitored through regular PSA tests, digital rectal exams, and occasional biopsies.
- Surgery: Prostatectomy involves the surgical removal of the prostate gland and surrounding tissues. It’s often recommended for localized prostate cancer, aiming to remove the tumor entirely and potentially cure the disease.
- Radiation Therapy: Utilizing high-energy radiation beams to target and destroy cancer cells in the prostate. External beam radiation therapy (EBRT) and brachytherapy are common approaches. EBRT delivers radiation from outside the body, while brachytherapy involves placing radioactive seeds directly into the prostate.
- Hormone Therapy: Also known as androgen deprivation therapy (ADT), hormone therapy aims to reduce levels of male hormones (androgens) like testosterone, which can fuel the growth of prostate cancer cells.
- Chemotherapy: While less commonly used as a first-line treatment for prostate cancer, chemotherapy may be recommended for advanced or metastatic prostate cancer that has become resistant to hormone therapy. Chemotherapy drugs are administered intravenously or orally, circulating through the bloodstream to target and kill cancer cells throughout the body.
What’s the Difference Between BPH and Prostate Cancer?
BPH and prostate cancer are two distinct conditions that affect the prostate gland in men. Here are the key differences between BPH and prostate cancer:
Cell Growth
BPH results from an overgrowth of prostate cells, leading to an enlargement of the prostate gland. Unlike BPH, prostate cancer involves the uncontrolled growth of cancerous cells, and it has the potential to spread to other parts of the body.
Disease Progression
BPH is generally a slow, progressive condition. While, prostate cancer can vary in aggressiveness, with some forms being slow-growing and others more rapidly advancing.
Risk of Cancer
BPH is a non-cancerous enlargement of the prostate gland. It is a common condition that occurs as men age, and it is not associated with cancer. Prostate cancer, on the other hand, is a malignant tumor that develops in the prostate gland.
Treatment Approach
BPH focuses on managing symptoms and improving quality of life, while prostate cancer treatment aims to eliminate cancer cells and prevent a recurrence.
BPH Diagnosis and Treatment at American Prostate Centers
While both BPH and prostate cancer can cause urinary problems, it’s important to remember that they are distinct conditions with different prognoses and treatment options. Early detection is crucial for both. If you experience any concerning symptoms, don’t hesitate to schedule an appointment with one of our prostate specialists for a proper diagnosis and personalized treatment plan.